In the last few decades, the microscopic parasites that cause the deadly malaria disease have been developing partial resistance to the antimalarial drugs that save lives. The development of this partial drug resistance, while caused by the smallest of genetic adaptations in the disease-causing plasmodium falciparum parasites, could have the largest of impacts on global public health.
Consequently, these teeny organisms have stimulated some big questions in the field of genomic malaria research–questions that may require one of the world’s most powerful supercomputers to solve. And that’s exactly what graduate student Cecile Meier-Scherling plans to do.
Cecile Meier-Scherling, a rising 4th-year graduate student in Brown CCMB’s Computational Biology PhD program, was recently awarded the Frontera Computational Science Fellowship, a one-year fellowship that will give her access to use Frontera, the fastest supercomputer at an academic institution in the United States, for her work in computational malaria research.
The Frontera Fellowship provides graduate students in a multitude of disciplines with the opportunity to carry out their computational research on the supercomputer and receive mentorship from experts at the Texas Advanced Computing Center, where the supercomputer is housed at the University of Texas, Austin.
Cecile is one of the six students from across the country who have been awarded the Frontera fellowship and will be using the supercomputer in the next year. She will be studying the DNA of the malaria parasite and trying to learn more about the genetic differences between the parasites in East and West Africa, where drug-resistance has recently been accelerating.
Malaria is an interesting disease for a lot of reasons, but for Cecile, it's the computational challenges associated with trying to understand it that drew her to this field. Though she had previously been doing cancer research, Cecile’s rotation with malaria researcher Jeff Bailey during her first year at Brown sparked a new interest: “With malaria, you work with much sparser data and smaller data structures. Because of this, malaria presents really interesting computational problems.”
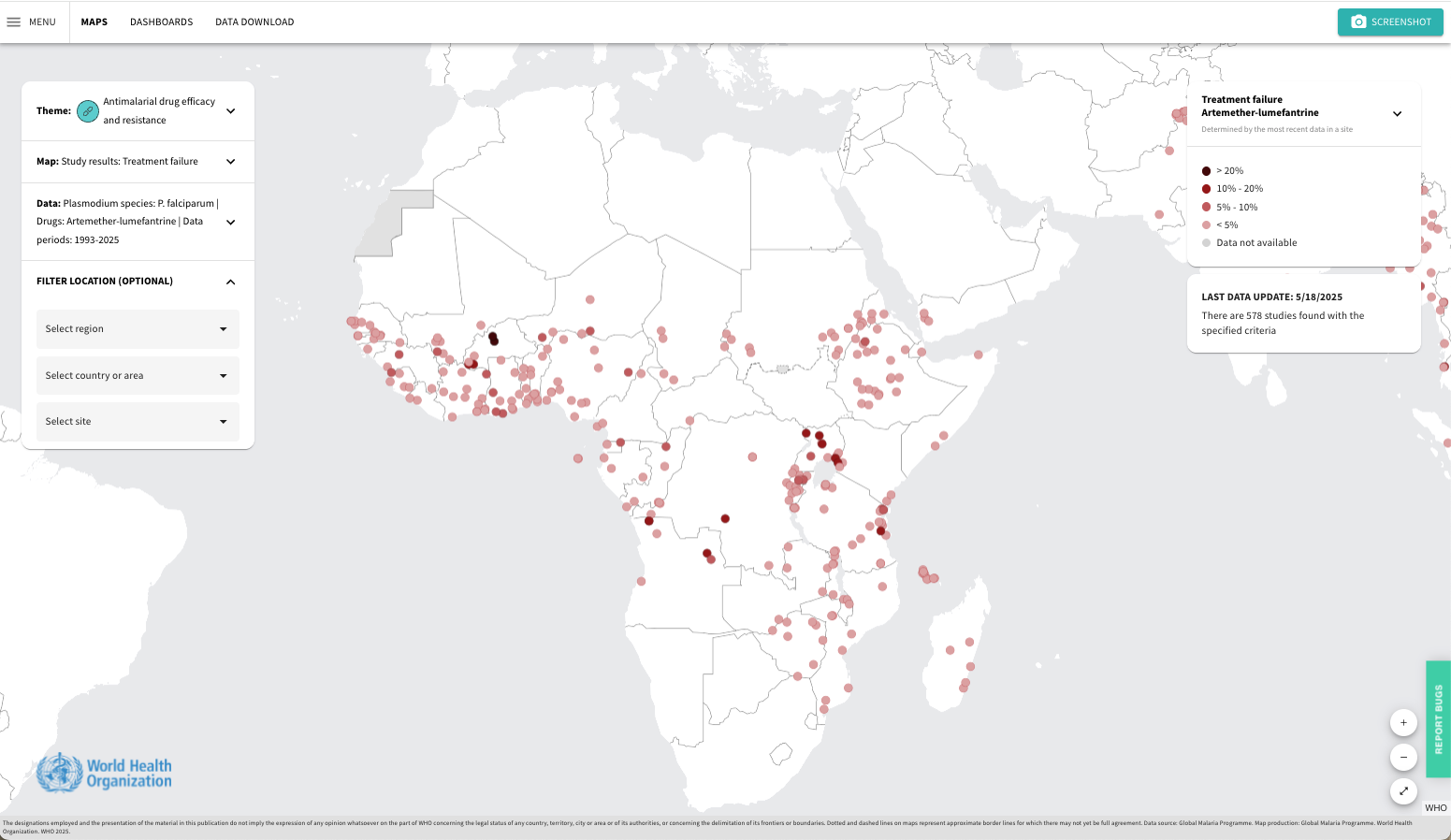
Three years in, Cecile now uses machine learning and probabilistic modeling to study malaria in two main ways: by looking at the dynamics of the spread of anti-malarial drug resistance across time and space, and by analyzing the genome of the malaria parasite to understand how this drug-resistance may be developing genetically. Cecile’s line of research is made particularly difficult by the fact that parts of the parasite’s genome are “unmappable.”
Essentially, in order to study the new adaptations in the parasite’s DNA that have allowed partial drug-resistance to develop, researchers like Cecile need to compare the resistant DNA to what is called the “reference genome” for the malaria parasite. A reference genome is the basic blueprint for what a particular species’ DNA should look like, and it is put together by studying numerous examples of a particular species’s DNA and figuring out what they all have in common.
However, for the plasmodium falciparum parasites that cause malaria, it turns out that there is so much genetic variation among individual organisms within these “unmappable” parts of their genome that it’s impossible to figure out what the reference genome should look like in the first place.
“These unmappable regions of the genome are of particular interest because they harbor the genes that help the parasites evade human immunity,” says Cecile. Because there is no ground truth genomic model to which we can compare parts of the parasite DNA, it makes it really hard to develop new vaccines and drugs that target the ability to evade human immunity. Luckily, researchers like Cecile have a tool that might help them understand these unmappable regions a bit better.
“There’s a computational tool that was developed out of Stanford that uses a statistical approach to understand what the potential genetic variations of unmappable regions could be,” says Cecile, which would help researchers get a better idea of how the unmappable regions are structured and how they impact drug-resistance.
So far, this computational method has only been tested on the genomes of prokaryotes–organisms made of single cells that do not have nuclei. Contrastingly, plants, animals, and the plasmodium falciparum parasites alike are eukaryotes: multicellular organisms whose DNA can have a lot more genetic variation within a single species than their single-celled cousins. With the computing power of the Frontera supercomputer, Cecile plans to figure out how to adapt this computational method to study the genome of the malaria parasite.
Cecile’s work will help researchers understand the parasite’s opaque genomic regions a bit better, which will in turn hopefully reveal important geographical differences between the parasites. “Right now, the parasites within East and West Africa look pretty similar with the current information we have,” says Cecile. “The question is, what if we add this information that we currently cannot access; then can we get a more granular view that will help us identify the differences between different parasite populations?” The hope is that understanding the differences in parasite populations will help researchers identify regions of the genome that would be particularly suitable for novel drug and vaccine targets.
Following this line of inquiry and thinking about the future directions of her research, Cecile is intrigued by the applications of her work in drug development. “I’m really interested in using the tools I’ve built, these mathematical models and machine learning tools, in identifying early drug targets, especially for small-data diseases” she says. “Identifying new candidates for successful drugs or developing the next iterations can be very labor intensive and expensive, so I want to learn how we can use modeling to optimize drug development.”
With the Frontera Fellowship, Cecile is getting to meld together her research interests in population genetics, genomics, and computational methods design. “I’m super excited about these opportunities and having the support to pursue this research,” says Cecile. “Getting to collaborate with new folks and experience new places like Austin is going to be great.”
The computational and medical challenges of malaria are bound to grow as drug-resistance slowly spreads. But Cecile Meier-Scherling, with her boundless enthusiasm and her foot in many doors, is ready to continue tackling these troublesome parasites.


